What are the best clinical communication tools?
NHS communications issues in England cost the taxpayer upwards of £1 billion per year. Not only could these funds be better spent improving healthcare outcomes for patients, a lack of effective communications (including quality and accuracy of information) is one of the leading reasons for hospital complaints and patient safety issues.
However, despite increases in funding across the NHS to integrate digital solutions into everyday operations, the reality remains that NHS staff are having to use tools like paper, bleeps, phone calls, and instant messaging apps like WhatsAppto manage clinical communications and coordinate, track, and document patient care.
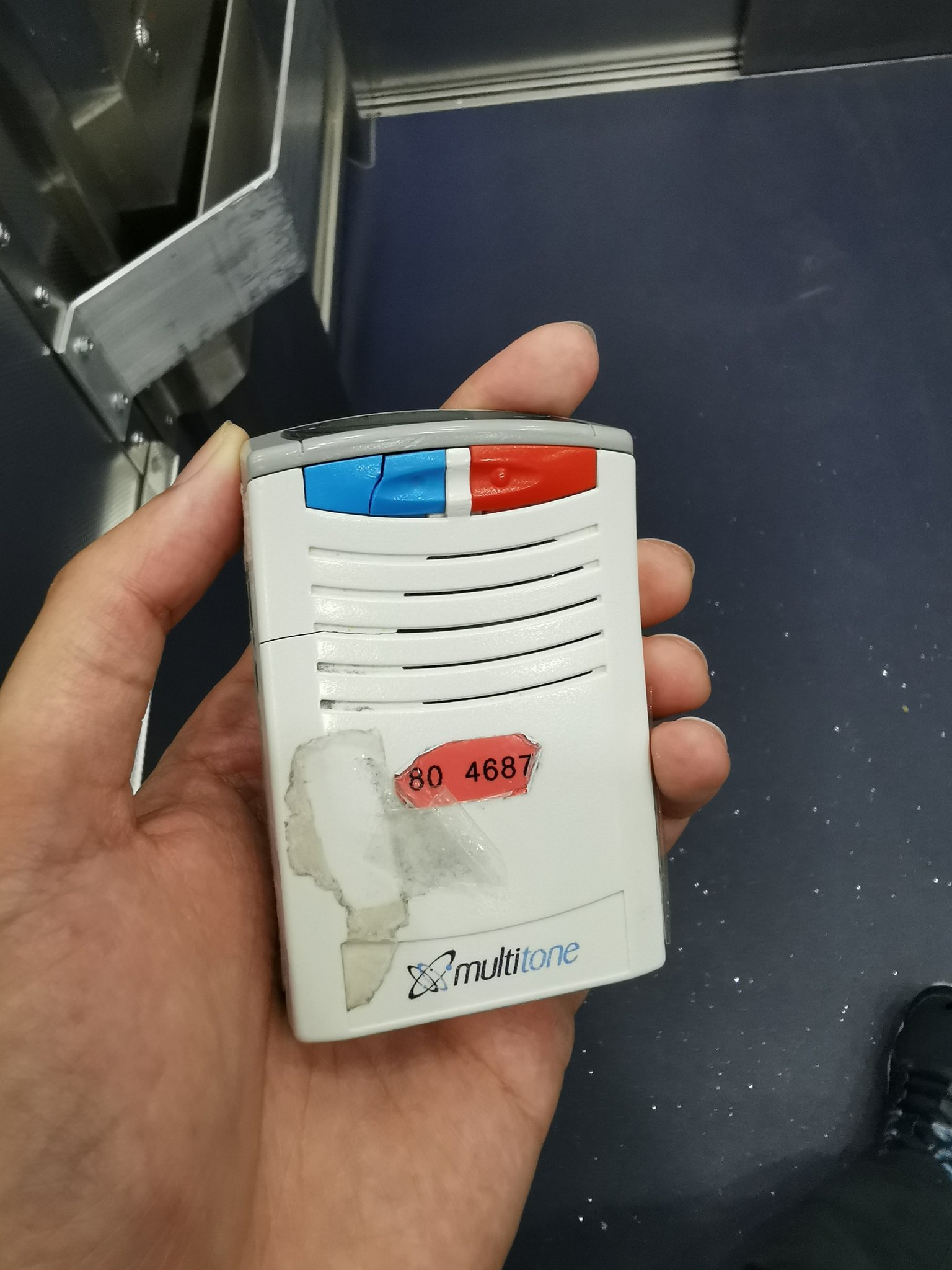
Outdated clinical communication tools
These outdated tools make it difficult to share information, create inefficiencies, and can even contribute to harm. Paper, bleeps, and phone calls may not be expensive, but they can be costly in other ways – lack of visibility and time pressures mean avoidable incidents inevitably result from using them.
An example of an NHS critical care handover sheet, which requires the user to hand-write notes throughout their shift
Regardless of the NHS clinical communication tools used, staff often add information gathered to a paper “to-do” list, which they carry around throughout their shift, adding items as they go. This has many safety and information security risks, and can’t be easily shared with the team unless staff are physically in the same location.
What already exists?
Electronic Health Records (EHRs) are in widespread use across the NHS, but most of them are not set up for mobile task management. EPRs are often not user-friendly, staff may have to log in to multiple systems to get information, and there can be an “information overload” when just the pertinent information is needed at the point of care. Additionally, EPRs don’t allow staff to easily share information with their team members, which can make real-time management of patients challenging.
Other industries have adopted task management tools with success, but they are simply not fit for the complexities of health and care. The use of spreadsheets is also inadequate for healthcare, and with large numbers of staff across multiple teams needing access, can quickly become a risk to patient safety.
Messaging tools allow staff to share information, but tasks or requests are almost always added by hand to one or more paper lists that staff carry in their pockets during their shift. It’s a workaround, which helps to support the outdated and unsafe practice of managing health and care tasks using paper, bleeps, or spreadsheets.
Understandably, staff are calling for an upgrade to NHS communications and collaboration tools. They need solutions that are real-time, auditable, and inherently multidisciplinary, allowing all healthcare professionals to safely and efficiently care for patients. Better tools will also support their workload management and reduce stress and burnout.
So what does the ideal NHS clinical communication tool look like?
A safer, easier, alternative
NHS communications are often about “tasks”
In hospitals, team handover meetings happen usually 12-hourly, when the previous shift ends and the new shift begins. Handovers must ensure that the incoming team understand what has been done for patients already and what needs to be done for them going forward - “tasks” of caring.
In the past, each attendee to a handover would make a handwritten list, and every member of staff would maintain their own copy. Now, usual practice is that staff have a printed document or spreadsheet, which they add to (by hand, often) during their shift. They then handover again at the end of their shift, and add relevant information to the Electronic Health Record. In between handovers, new information about tasks is not easily shared with team members, which necessitates staff to communicate via text, instant message, phone call, bleep, and in-person.
At its core, the real issue with NHS clinical communication tools is a lack of a shared, real-time repository of information about patients and the tasks required to treat and care for them. A “digital to-do” list which shows all patients within a service, that relevant multidisciplinary staff can access and add to at any time.
A real-time, shared, task list
If health and care staff had a real-time patient and task list that they could access and update from anywhere for their colleagues to see, they wouldn't need to rely so heavily on a range of manual, time-consuming, and outdated methods to get and share the information they need.
Infinity is such a tool. It improves NHS clinical communication and collaboration, connecting team members virtually, and enables them to access real-time information about tasks from anywhere.
With Infinity, staff don’t need to send a text or instant message about Patient A on Ward 3 needing Y treatment within a certain timeframe, hoping that their request is seen by the right person, written down, and actioned. They can add the task to the digital list, assign it to an individual or role, and instantly see when it has been accepted, started, and completed.
Likewise, staff can be allocated tasks to their own list and mark their progress for others to track. This also allows senior staff to have activity of their team and support them. Staff have access to everything they need from wherever they are, and at any time.
Clinical teams can immediately see and act on new information
At London North West University Healthcare NHS Trust for example, staff in the early supported discharge and rapid response community team are using Infinity’s clinical communication and collaboration tool to add new tasks to their patient list, check off the tasks they have completed for their colleagues to see, and more easily and safely organise their days.
“Using Infinity has improved our team’s communication – it’s a lot easier to keep in contact about tasks for the day. Things change all the time, so it’s great to be able to add tasks to the platform and know the clinical team will be able to see and act on it immediately from a visit, without having to call, email, or text them.”
- Team Leader
London North West University Healthcare NHS Trust
Not only has the department seen an improvement in ease of communication, Infinity is saving more than eight person-hours per day - in travelling to and from patients, in calling, in emailing, in texting, in instant messaging. It’s helping some clinicians to see 1-2 more patients each every day - a capacity increase of up to 55% - and it’s making sure staff can easily see tasks that they may have missed.
It’s now up to the NHS to turn to a new generation of clinical communication and collaboration tools and start to solve its £1 billion communications problem. Not only to save money, but also to boost clinical safety, patient flow, and staff welfare.
If you want to get to the root of clinical communications issues within your organisation - NHS or other health and care - please get in touch by emailing [email protected] - we’d love to help.